Diphallus, which is also known as diphallia, is a very rare congenital anomaly encountered nearly one in 5.5 million population. Since the first case was presented by Wecker in 1609, only 120 cases have been reported in the literature so far. Vast majority of cases with diphallus were accompanied by various congenital anomalies mainly genitourinary and anorectal malformations. Diphallus can be classified as glandular diphallus, bifid diphallus, and complete diphallia according to the anatomical structure involved.
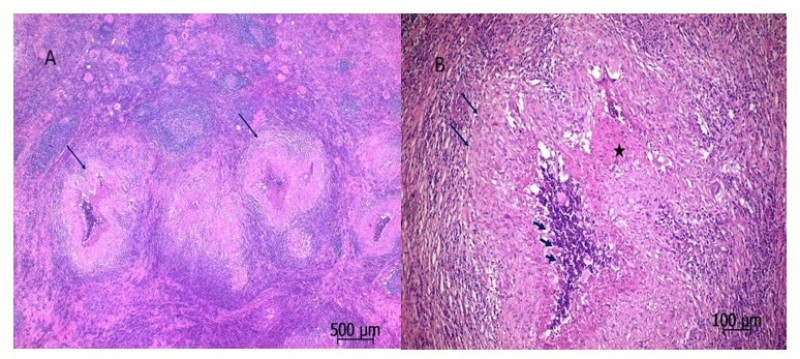
Cat scratch disease (CSD) is a self-limiting infectious disease that develops after a cat bite or scratch, caused by the Gramnegative bacillus Bartonella henselae []. It is seen in children, young adults, patients with compromised immune systems, and rarely in the elderly []. The disease is generally characterized by fever and regional granulomatous lymphadenopathy, but it can occur as a systemic disease in 5-10% of cases and lead to various diseases []. In systemic CSD, all systemic organs, especially the liver and spleen, can be affected along with longterm fever [].
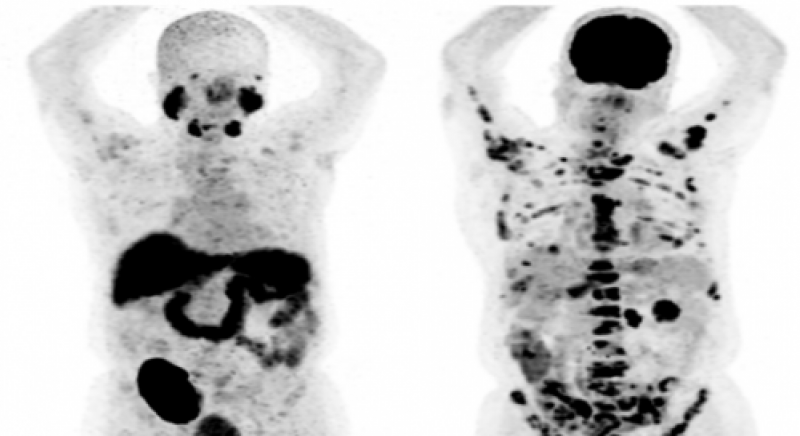
Immunosuppressive therapy is related to the increasing frequency of malignancies after transplantation. A small percentage (4.6%) of malignancies seen in kidney transplant patients are renal cell carcinomas (RCC) which occur almost exclusively in native kidneys. The prognosis of RCC largely depends on the presence of metastasis. Metastatic disease is very rare in small renal masses. In this case report, we aimed to present our case of approximately 4 cm-mass of metastatic RCC in our kidney transplant patient.
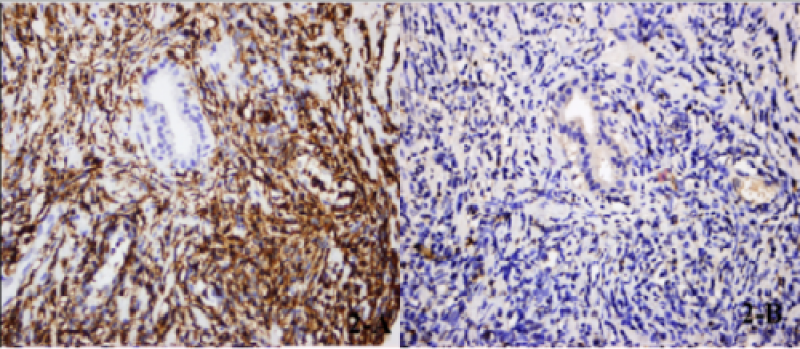
Primary or secondary lymphoma of the prostate is a rare condition. Mantle cell lymphoma (MCL) represent 4-9% of all lymphomas. Prostate involvement with MCL is very rare, with only 11 reported cases up to now. Here we present a case with lower urinary tract symptoms and prostate-specific antigen (PSA) elevation diagnosed with MCL of the prostate. Prostate biopsy was performed in a 70-year-old patient due to increased PSA. After the pathology result was reported as prostatic MCL, imaging studies and sampling of additional pathological specimens were performed for staging. 488 576

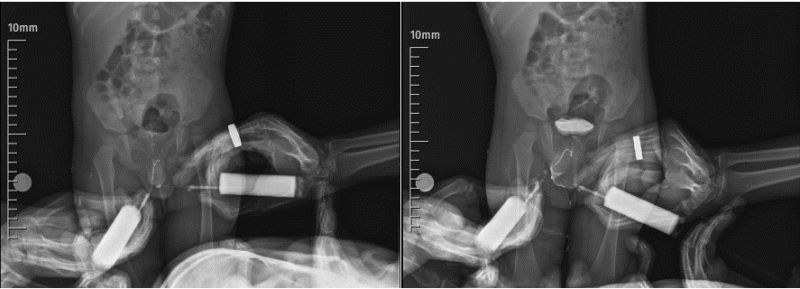
Apparently, genetic factors, especially in oligoospermic and azoospermic patients, have been increasingly investigated in recent years. Klinefelter syndrome (KS), known as 47XXY, can be seen in up to 10% of the cases with nonobstructive azoospermia and in one in 500-1000 live births [4]. Various variants of Klinefelter syndrome have been reported. Here, a case with a genetic diagnosis of 48XXYY, which is a very rare variant of Klinefelter syndrome, will be presented.