A 50-year-old male patient was admitted to our emergency
department with the complaint of prolonged erection lasting for
about three hours without sexual stimulation. As understood
from the patient's anamnesis and medical file, he applied
to the emergency department with the complaints of fever,
lassitude, and fatigability in 2015. His hemogram parameters on
admission were: WBC:18.2 x109/L, Hgb: 12.9 g/dl, Htc: 39%,
PLT: 379 x103 K/μL. Besides, his lactate dehydrogenase (LDH)
and uric acid values were elevated were found to be high, and
he was referred to the hematology clinic with a preliminary
diagnosis of leukemia. In the physical examination, any
remarkable finding other than splenomegaly was not detected.
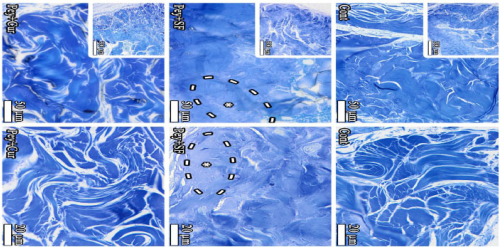
Microscopic examination of his peripheral blood smear revealed
the presence of platelet deformities, megakaryocyte fragments,
normocytic normochromic erythrocytes, all cells of myeloid
series, markedly increased number of basophils and eosinophils,
myelocytes, metamyelocytes, rods and fragmented neutrophils.
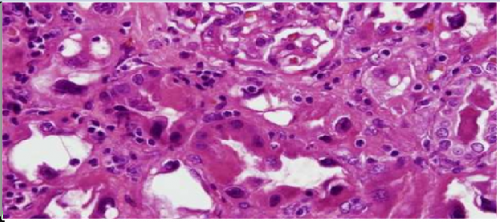
It was learned from his medical documents that the patient
received the diagnosis of "CML in chronic phase" based on
the histopathologic examination reports of the bone marrow
aspiration and biopsy specimens obtained for definitive diagnosis,
Karyotype analysis revealed the presence of Philadelphia (Ph*)
chromosome, and BCR/ABL chimeric gene was detected using
PCR and FISH techniques. The patient diagnosed with CML
received initial treatment with single daily oral doses of a firstgeneration
tyrosine kinase inhibitor (imatinib 400 mg cap.) and
allopurinol (300 mg tb) and he was called for outpatient control.
The patient, who claimed that severe muscle and bone pain
developed during the imatinib treatment stopped taking the drug
by his own decision, so hematology physician started to give him second generation tyrosine kinase inhibitors in turn (nilotinib
and dasatinib). However, it was observed that these drugs also
caused severe pancytopenia, and treatment with single daily oral
doses of 400 mg imatinib was started again. Still, it was noted
that the patient used the drug irregularly, stopped using the drug
from time to time and did not routinely attend the hematology
outpatient clinics for control.
The patient stated that he had been prescribed trazodone
HCl (50 mg/d PO) in another center due to the anxiety he had
experienced and had taken the first dose the previous evening.
The patient said that he had never experienced a spontaneously
prolonged erection before and thought that the cause of the
problem developed was related to trazodone tablet he had used
for the first time the previous evening. From the anamnesis
of the patient, it was learned that he did not use any drugs
containing phosphodiesterase-5 (PDE-5) inhibitors. The results
of the hemogram test performed when the patient applied to our
emergency department were as follows; WBC: 22.2 x109/L,
Hgb: 10.9 g/dl, Htc: 30%, and PLT: 579 x103 K/μL. The patient
was admitted to the urology clinic for examination and treatment
because of the sustained rigid erection. As the first intervention
performed in the urology clinic, an 18G butterfly needle was
inserted laterally into both penile corpora cavernosa of the
patient to aspirate cavernosal blood. When the erection persisted
despite aspiration, intracavernosal irrigation with 0.90% w/v
saline was performed, but when detumescence could not be
achieved, intracavernosal injection of 2 ml 1/100,000 adrenaline
was performed. After the procedure, detumescence was ensured,
a CobanTM self-adherent bandage was wrapped around the
penis to prevent development of hematoma. The patient was monitorized for 4 hours, and then discharged. Priapism did not
occur again during the follow-up period.
Chronic Myeloid Leukemia (CML) is a stem cell disease
manifested by abnormal clonal proliferation of myeloid
precursor cells and accounts for 15% of adult leukemias. Its
incidence is 1-2/100,000. It is more common in men (male/
female: 1.3/1) and its incidence increases between the ages of
40-60. CML was the first disease in humans to be associated
with a specific chromosomal abnormality. In more than 90% of
CML cases, the Philadelphia (Ph*) chromosome is detected by
cytogenetic analysis [,].
Symptoms associated with anemia (such as weakness, fatigue,
effort intolerance, decreased functional capacity), splenomegaly
(abdominal swelling and pain, rapid satiety due to pressure of
enlarged spleen on the stomach) hypermetabolic state (fever,
anorexia, weight loss, gout), platelet dysfunction (hemorrhage,
ecchymosis, hematoma, thromboembolic events, retinal
hemorrhage), hyperleukocytosis and hyperviscosity-related
findings (tinnitus, stupor, visual impairment, dyspnea, priapism
and cerebrovacular events), thrombocytosis, hypereosinophilia,
increase in basophil counts, anemia, elevated LDH and uric acid
levels can be seen in CML. Physical examination reveals the
presence of splenomegaly in 50-90%, and hepatomegaly in 10-
20% of CML patients [,].
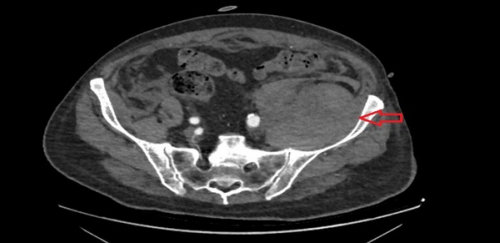
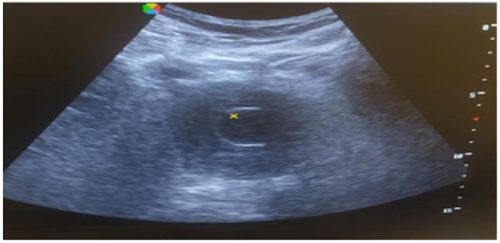
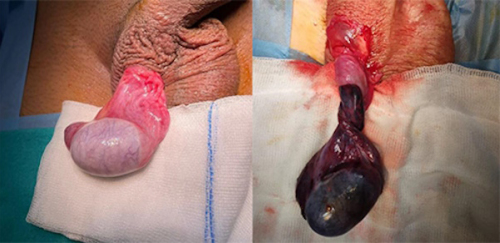
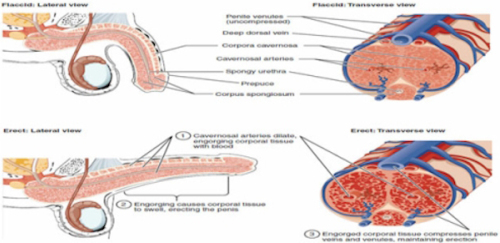
Priapism is an uncontrolled, prolonged, and sustained
erection developing without sexual stimulation and cannot be
terminated by ejaculation, (Figure 1). This is a true urological
emergency and early intervention is crucial for functional
recovery. It has ischemic, non-ischemic and intermittent
subtypes. Although often idiopathic priapism is seen, many
etiologic factors of priapism are known including hematological
diseases (ie. sickle cell anemia, thalassemia, leukemia, multiple
myeloma), toxins (ie. scorpion, spider, malaria), metabolic
diseases (ie. Fabry disease, amyloidosis), neurogenic diseases
(ie. brain tumors, cerebrovascular diseases, spinal cord injury),
metastatic or local invasion of tumors (ie. prostate, urethra, testis,
lung) and drugs (PDE-5 inhibitors, vasoactive erectile agents
such as papaverine, alpha adrenergic receptor agonists, heparin,
warfarin, antidepressants, antipsychotics, antihypertensives,
testosterone, alcohol, and cocaine) [].
Figure 1. Top: Flask penis, Bottom: Erect penis
Corporeal relaxation exerts external pressure on the emissary veins emerging from the tunica albuginea, causing blood to remain in
the penis resulting in an erection. https://storymd.com/journal/mpq5pdku6j-penis/page/elqozasy75pq-penis
Imatinib mesylate is the first selective tyrosine kinase
inhibitor (TKI) to target the BCR-ABL protein. While nilotinib
and dasatinib are second generation tyrosine kinase inhibitors
used in the treatment of imatinib-resistant CML. Muscle cramps,
joint, muscle or bone pain, which are common imatinib-related
side effects, may also occur during imatinib treatment or after its
discontinuation [].
Trazodone HCl is an antidepressant used in the treatment of symptoms caused by anxiety and depression such as anxiety,
appetite disorder, insomnia, and attention deficit. Serotonin
reuptake inhibitors (SSRIs) belong to the drug group and its
most basic feature is that their effects start to improve symptoms
within a short period of about a week.
In addition to common side effects such as blurred vision,
headache, dizziness, and severe fatigue, long-term painful
erection (not associated with sexual activity) may also occur
in men when using trazodone HCl []. Although the relevant
mechanism is not fully understood, its high affinity for the α1
and α2 receptors that trazodone antagonizes is blamed in the
pathophysiology []. This antagonism causes an increase in
blood flow due to arteriolar dilation followed by a decrease in
venous flow and obstruction of the emissary veins. In addition,
α1 blockade may trigger nitric oxide release in nerves innervating
arterioles and corpora cavernosa []. This whole process results
in an erection.
CML is one of the etiologies of priapism and there are
multiple relevant case reports in the literature [,]. Herein, it
has been accepted that priapism develops due to stasis associated
with leukocyte aggregation in the corpora cavernosa and penile
dorsal vein due to hyperleukocytosis. Another contributing factor
to venous occlusion is the mechanical effect of pressure from the
abdominal veins draining the spleen. In addition, infiltration into
the sacral nerves or central nervous system by leukemia cells is
thought to contribute to the process [].
In our case, remission of the disease could not be
achieved because the patient did not regularly use tyrosine
kinase inhibitor (TKI) drugs that regulate the leukocyte level of
the patient. Despite hyperleukocytosis and hyperviscosity in the
bloodstream, which are considered to be the causes of priapism
in CML, the patient did not develop priapism. However,
priapism, which cannot develop on the basis of CML alone,
has been predicted to develop due to the synergistic effect of
antidepressant agent trazodone HCL in the pathogenesis.
Ethics Committee Approval: N / A.
Informed Consent: An informed consent was obtained from
the patient.
Publication: The results of the study were not published in full
or in part in form of abstracts.
Peer-review: Externally and internally peer-reviewed.
Authorship Contributions: Any contribution was not made by
any individual not listed as an author. Concept – S.I.G.; Design
– S.I.G.; Supervision – S.I.G., E.G.; Resources – D.N.O.;
Materials – D.N.O.; Data Collection and/or Processing –
S.I.G., D.N.O.; Analysis and/or Interpretation – S.I.G., D.N.O.;
Literature Search – D.N.O.; Writing – S.I.G.; Critical Review
– S.I.G., E.G.
Conflict of Interest: The authors declare that they have no
conflict of interest.
Financial Disclosure: The authors declare that this study
received no financial support.