Objective: Benign prostatic hyperplasia (BPH)-related acute kidney injury (AKI) occurs in male patients as a natural result of aging and androgen exposure. In our study, we investigated the frequency of BPH-related AKI and its relationship with disease severity in patients hospitalized for COVID-19 pneumonia.
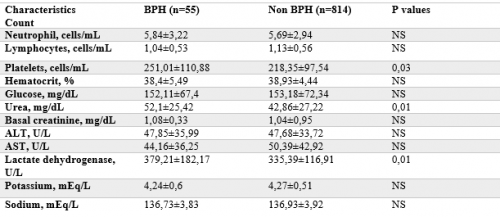
Materials and Methods: This is a retrospective and observational study on 869 male patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), who were diagnosed with COVID-19 by real-time PCR testing and hospitalized due to COVID-19 pneumonia. None of the patients was admitted to the intensive care unit (ICU). 55 patients out of 869 had BPH. AKI was defined according to Kidney Disease: Improving Global Outcomes (KDIGO) criteria. BPH and non-BPH groups were statistically compared with respect to the existence, frequency, hospitalization duration and in-hospital death.
Results: Median age was 70 years for BPH group and BPH patients were significantly older than the non-BPH. Hypertension, coronary artery disease and heart failure were significantly more frequent in the BPH group. On admission, compared with normal serum creatinine, serum urea was significantly higher in the BPH patients. All AKI patients with BPH had three or more comorbidities. During hospitalization, AKI occurred in 7,3% of the BPH patients compared with the non-BPH (0,98%). The incidence of AKI was significantly higher in the patients with BPH (OR:7,94, 95% CI:2,31-27,25). In-hospital death occurred in 16,4% of the patients with BPH. The mortality was significantly lower in non-BPH group (8,6%) compared with the BPH. Our final analysis showed that age, arterial hypertension, prior coronary artery disease and heart failure were independent risk factors for occurred BPH-related AKI.
Conclusions: Older male patients with common comorbidities showed a higher risk for mortality from COVID-19 pneumonia. Also, AKI patients with BPH had a poorer prognosis and higher mortality than the non-BPH patients.