A 55-year-old female patient admitted to the emergency
department with one week long abdominal pain. In the physical
examination of the patient, no clinical finding other than
sensitivity was observed. The laboratory tests were normal.
Because there was discordance between the patients clinical
findings and laboratory tests, ultrasound exam was performed
to exclude acute abdomen and a mass was detected in the
anterior of left kidney's upper pole. There upon, the patient was
discharged with recommendations and directed to the urology
department. The patient had no history of malignancy or surgical
history. Contrast enhanced abdominal magnetic resonance (MR)
was performed for the lesion characterization. In the abdominal
MRI, a lesion was detected in the anterior region of the left
kidney's upper pole which is 36x20 mm in size. The lesion was
hypointense on T2 weighted images (WI), slightly hyperintense
on T1WI and had central cystic area. Since the mass was closely
adjacent to the tail of the pancreas and had similar signal intensity
with the pancreas on T2WI and postcontrast images, the origin of the lesion could not be made clearly between left kidney
and pancreatic tail (Figure 1-5). Therefore, histopathologic
verification was recommended for preoperative management.
It was reported as angiomyolipoma, wihch is rich in smooth
muscle and poor in fat, after staining with actin and HMB-45
along with immunohistochemical staining obtained as a result
of the biopsy procedure.
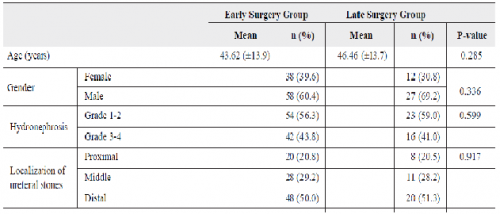
Figure 1: Axial T2 weighted (Contrast-enhanced
abdominal magnetic resonance images of the patient)
Figure 2: In phase (Contrast-enhanced abdominal
magnetic resonance images of the patient)
Figure 3: Out of phase (Contrast-enhanced abdominal
magnetic resonance images of the patient)
Figure 4: T1 Weighted, fat saturated T1
weighted (Contrast-enhanced abdominal
magnetic resonance images of the patient)
Figure 5: Post contrast images revealed
a solid mass with central cystic area
(Contrast-enhanced abdominal magnetic
resonance images of the patient)
Renal angiomyolipomas are the most common benign kidney
tumors. Non invasive diagnostic capacity between benign and
malignant lesions is not yet at the desired standard. Approximately
10-17% of the resected kidney tumors are benign, and 2-6% of
them are reported as angiomyolipomas []. Angiomyolipomas
contain smooth muscle tissue, blood vessels and macroscopic
fat areas in varying proportions []. In most cases, it is
diagnosed radiologically without any further examination due
to the macroscopic fat content. In the radiological diagnosis of
angiomyolipoma, we use findings such as containing densities
below -10 HU in computerized tomography (CT) examination or showing suppression in fat saturated sequences in MRI [].
In addition, chemical shift suppression techniques are useful in
MRI in cases when there is a small amount of fatty tissue [].
On the other hand, in 4.5% of angiomyolipomas, fatty tissue
may not be seen radiologically []. Since the imaging findings
of these fat-poor lesions, containing less than 25% fat, cannot
be distinguished from RCC and they pose a serious problem
[]. RCCs, especially clear cell carcinomas, may also contain
fat, but unlike angiomyolipomas, this adipose tissue is located
at intracellular space and we use signal loss in out of phase
MR sequence to differentiate RCC from angiomyolipoma [].
Angiomyolipomas carry the risk of bleeding, especially in sizes
over 4 cm and sometimes, fat densities can be overlooked due to
intralesional bleeding and they can be confused with RCC [].
Although new methods such as CT histogram [] and specific
MR sequences [,] have been used in the separation of fatpoor
angiomyolipoma and RCC with new developments in
radiology and technology, the application and reliability of these
methods in daily practice are not sufficient.
Ethics Committee Approval: N/A.
Informed Consent: An informed consent was obtained from
the patient.
Publication: The results of the study were not published in ful
lor in part in form of abstracts.
Peer-review: Externally peer-reviewed.
Conflict of Interest: The authors declare that they have no
conflict of interests.
Financial Disclosure: The authors declare that this study
received no financial support.