Objective: Recently, many hematological parameters have been frequently investigated as
prognostic and predictive biomarkers for malignancies and inflammatory conditions, with the
primary examples of these parameters being neutrophil-lymphocyte ratio (NLR), lymphocytemonocyte
ratio (LMR), platelet-lymphocyte ratio (PLR), and mean platelet volume (MPV). In
this study, we aimed to investigate the relationship between hematological parameters and
prognosis in patients with a diagnosis of testicular malignancy (TM) by evaluating them in
comparison with patients that underwent varicocelectomy as a control group.
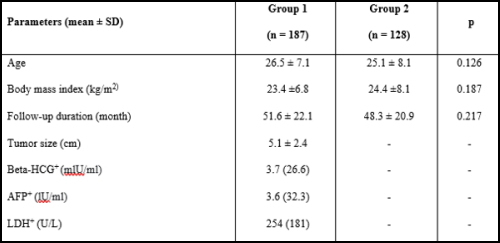
Materials and Methods: A total of 187 patients that underwent radical inguinal orchiectomy
due to the diagnosis of testicular tumor were included in Group 1and 128 patients of similar
age that underwent varicocelectomy using a similar incision in Group 2 as controls.
Hematological and biochemical blood results were collected one day before radical
orchiectomy. The parameters of NLR (neutrophil/ lymphocyte counts), PLR (neutrophil/
lymphocyte counts), PLR (platelet/ lymphocyte counts), and LMR (lymphocyte/ monocyte
counts) were expressed as the ratios of indicated blood cell components. Following standard
inguinal radical orchiectomy, T staging was performed based on the final histology samples,
and clinical N and M staging using imaging modalities.
Results: The mean (± SD) ages of the patients were 26.5±7.1, and 25.1±8.1 years for Groups 1
and 2, respectively. The neutrophil counts, NLR, and PLR were significantly higher in Group
1, while the lymphocyte count, MPV, and LMR were significantly higher in Group 2 (pT1 stage TM (pT1 in terms of MPV and PLR.
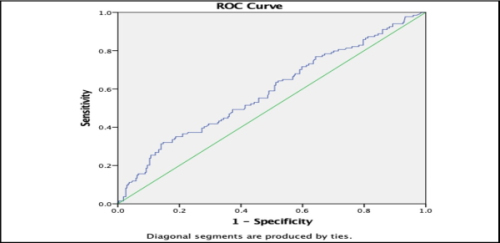
Conclusion: We determined NLR and LMR as parameters that can be used in the pathological
staging of cases with TM. We consider that these hematological parameters have an important
place in predicting the prognosis in this patient group.