A 22-year-old woman presented to the emergency
department with a 2-hour history of abdominal/flank pain. She
was involved in a motor vehicle collision where she was the
driver. Airbags were deployed, but her seat belt compliance
was unknown at the time of injury. Her medical history was
mysterious and unattainable due to her altered mental status. On
general appearance, the patient appeared intoxicated. Physical
examination was only significant for abdominal tenderness to
palpation. Vital signs revealed hypotension (97/64 mmHg). All
other values, such as pulse, temperature, oxygen saturation,
and respiration, were within normal limits. Laboratory values
on admission revealed elevated transaminases (AST 117/ ALT
86), and urinalysis showed hematuria (RBCs >182/HPF). All
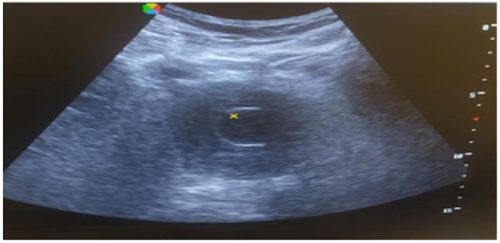
other values were within the normal range. A FAST (focused
assessment with sonography in trauma) ultrasound was
subsequently done, which revealed free fluid collection within
the abdomen.
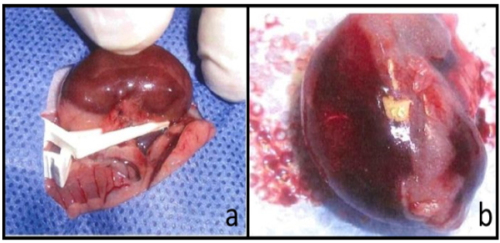
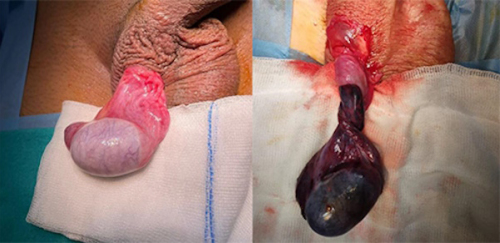
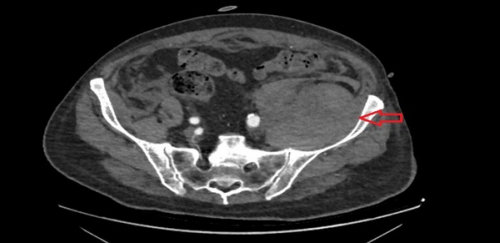
A multidisciplinary team, including urological surgery, was
consulted. A subsequent computed tomography (CT) scan of
the abdomen and pelvis showed intraperitoneal extravasation of
contrast, consistent with dome rupture (Figure 1). Exploratory
laparotomy was performed after and revealed a rupture across
the bladder dome (Figure 2). The bladder was surgically
repaired (3-0 Vicryl), and a Foley catheter was placed for
twelve days. On follow-up, a cystogram was performed, which
confirmed bladder healing, and the catheter was removed.
The postoperative course was uncomplicated, and the patient
completely recovered after two months.
Figure 1. A computed tomography scan of the pelvis
showing extravasation of contrast, which is consistent
with an intraperitoneal bladder rupture. A: coronal view;
B: sagittal view
Figure 2.
Laparoscopic
view of the
abdomen
demonstrating
free bloodstained
fluid in
the pelvic cavity
and rupture
across the dome
of the bladder
Bladder rupture is a rare condition due to the protection of the
bladder by the sturdy pelvic bones []. Today, bladder injuries
remain relatively uncommon, accounting for only up to 10%
of abdominal trauma [-]. Although motor vehicle collision is
the most common cause of injury, intragenic causes, including
surgical and endoscopic procedures, have also been identified [,]. Bladder rupture can be divided into intraperitoneal or
extraperitoneal rupture []. Extraperitoneal injuries are the most
common among the two, accounting for approximately 80% of
cases, with a general association of pelvic fracture with damage
to the bladder trigone, neck, or wall []. Extraperitoneal injuries
are commonly treated conservatively (with catheter drainage via
foley or suprapubic tube) []. Most bladder ruptures, regardless
of the classification, typically manifest with symptoms of
pelvic pain with difficulty voiding and gross hematuria [-].
Intraperitoneal injuries, on the other hand, account for 15%
of bladder injuries []. This typically occurs when there is a
compressive force against a full bladder, which ruptures the
weakest portion (dome) as presented in this patient [,]. A
FAST ultrasound may be positive as urine accumulates in the
abdominal cavity [,]. Treatment includes surgical repair,
which has demonstrated high success rates [-].
Recent practical guidelines regarding intraperitoneal bladder
injuries suggest surgical repair due to a more considerable risk for
lacerations with poor wound healing, electrolyte derangement,
and peritonitis [-]. According to the American Urological
Association (AUA) guidelines, extraperitoneal injuries should
be managed conservatively [-].
Acknowledgements: I would like to sincerely thank Dr.
Matthew Meece (Department of General Surgery, University
of Miami Leonard M. Miller School of Medicine/Jackson
Memorial Hospital, Miami, FL, USA) for his assistance in
interpretation of the images.
Ethics Committee Approval: Not applicable, as this is an
anonymous clinical image.
Informed Consent: The patient in this study provided written
informed consent prior to participation.
Publication: The results of the study were not published in full
or in part in form of abstracts.
Peer-review: Externally peer-reviewed.
Authorship Contributions: Any contribution was not made
by any individual not listed as an author. Concept – K.E.;
Design – K.E.; Supervision – K.E.; Resources – K.E.; Materials
– K.E.; Data Collection and/or Processing – K.E.; Analysis
and/or Interpretation – K.E.; Literature Search – K.E.; Writing
Manuscript – K.E.; Critical Review – K.E.
Financial Disclosure: This article received no specific grant or
support from any public or private agencies.