Objective: In this study, histological, pathological and clinical characteristics that may affect
multifocality rate and multifocality in renal tumors were investigated.
Materials and Methods: A total of 162 patients who underwent radical nephrectomy with
the diagnosis of renal tumor from our urology clinic and urology clinics in two other hospitals
between May 2002 and April 2006 and whose results were available were included in the
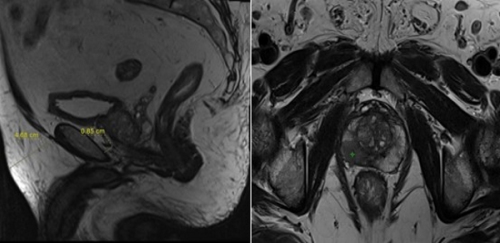
study. Kidney samples were evaluated regarding multifocality through sections made
macroscopically at an interval of 3 mm.
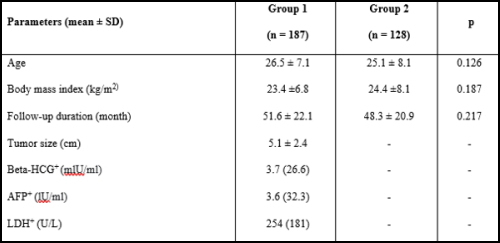
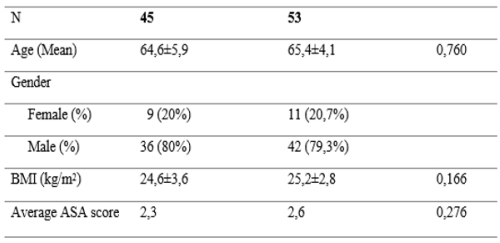
Results: Of the patients included in the study, 92 (56.8%) were male and 70 (43.2%) were
female. The mean age of the patients was 59.98 years (22-87). In 11 (6.7%) of 162 patients, a
multifocality focus was pathologically observed. Satellite lesions were radiologically
identified in two (18.2%) of the patients with multifocality. On the other hand, satellite
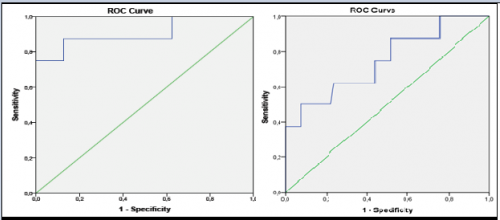
lesions could not be identified radiologically in nine patients (5.5%). Univariate and
multivariate analyzes were performed to determine the relation between pathological,
histological, and clinical characteristics and multifocality. There was no significant relation
between age, gender, smoking, the location of the tumor, pathological stage, lymph node
involvement, the presence of metastasis, the size of the tumor, and histology of the tumor.
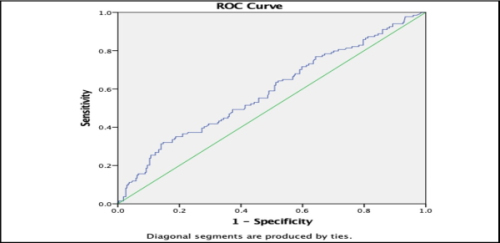
Univariate analysis results showed a statistically significant relation between renal capsule
involvement and renal vein involvement and multifocality (p=0.015 and p=0.004,
respectively); however, only renal capsule involvement was found to be associated with
multifocality in multiple logistic regression analysis (p=0.008).
Conclusion: In our multicentric study including 162 patients, the multifocality rate in renal
tumors was 6.7% (11 patients). There was a significant relationship between capsule
involvement and multifocality (p=0.015 – p=0.008). Meta analysis is required to determine
the rate of multifocality in renal tumors and identify with which clinical, pathological, and
histological characteristics it is associated.